Role of Human Menopausal Gonadotrophin for improving ovulation, fertility, and endometrial receptivity in PCOS women.

Infertility due to ovulation disorders is a leading reason for women to seek treatment1, with Polycystic Ovary Syndrome (PCOS) being the most frequent cause. PCOS aff ects 5%–15% of women depending on phenotype, ethnicity, and classification.2 It accounts for around 80% of anovulatory patients and is classified as a World Health Organization (WHO) group II disorder.3
The condition is characterized by chronic anovulation caused by endocrine and functional abnormalities, resulting in an imbalance of Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH) levels, which disrupts normal ovulation.3
Symptoms of PCOS include menstrual irregularities, infertility, increased androgen levels, insulin resistance, type 2 diabetes, obesity, hirsutism, and anovulation.3
The Rotterdam Consensus (2003) provides the most widely used diagnostic criteria, requiring two out of three features: oligo-ovulation or anovulation, hyperandrogenism, and polycystic ovaries on ultrasound. 4
Treatment for ovulation induction in PCOS ranges from lifestyle changes such as weight loss and exercise to medical interventions such as clomiphene citrate, aromatase inhibitors (letrozole), metformin, gonadotrophins, ovarian drilling, and in-vitro fertilization (IVF) for more resistant cases.4
Ovulation induction in PCOS
Ovulation induction is key for managing infertility in women with PCOS, involving both lifestyle and pharmacologic approaches. First-line therapy involves lifestyle modifications, such as weight reduction (targeting a BMI below 35 kg/m² or a 5%–10% bodyweight loss), which can restore ovulatory function and improve pregnancy rates. Clomiphene citrate remains the fi rst-line pharmacologic agent for inducing ovulation, though it carries a risk of multiple gestations. Aromatase inhibitors are an effective and
safe alternative, especially in obese patients. In cases of clomiphene resistance, metformin may be added to enhance ovulation, particularly in older women with central obesity. Second-line options include gonadotrophins, which necessitate close monitoring due to the risks of ovarian hyperstimulation syndrome (OHSS) and multiple pregnancies. For clomiphene-resistant patients, laparoscopic ovarian drilling (LOD) can be considered, though it poses risks such as reduced ovarian reserve. An IVF is indicated for patients who do not respond to gonadotrophins or have other IVF indications. Each treatment carries specific benefits, risks, and costs, requiring individualized patient management and counseling.4
Hormonal imbalances and anovulation in PCOS
In PCOS, high gonadotrophin-releasing hormone (GnRH) increases LH and the LH/FSH ratio, which boosts androgen production. Excess androgens cause follicles to stop developing, and high anti-Müllerian hormone (AMH) levels worsen this issue, leading to anovulation. The term “polycystic” is misleading as the small follicles seen are not true cysts. Obesity can worsen symptoms through insulin resistance and higher androgen levels. Treatments focus on reducing androgens and promoting follicle development to address infertility.2
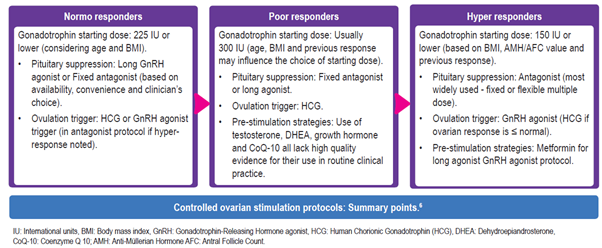
Controlled ovarian stimulation protocols: Summary
Ovulation induction is often one of the first strategies for managing infertility in women with a history of PCOS. When ovulation induction proves ineffective or fails, assisted reproductive technologies (ART) offer an alternative approach. IVF presents several challenges, including the risk of OHSS, elevated serum estradiol levels, and accelerated endometrial maturation. Additionally, strategies like freeze-all embryo policies are considered to address these issues. Choosing the optimal ovarian stimulation protocol is crucial for addressing these challenges.5
Clinical approach for inducing ovulation and treatinginfertility in patients with PCOS: HMG in various protocols
Xia T et al. assessed the effectiveness of three different ovulation induction therapies for treating infertility in women with PCOS. They compared the outcomes of 90 patients who underwent intrauterine insemination. These patients were randomly assigned to one of three treatment groups: letrozole combined with urinary gonadotrophin (HMG/human menopausal gonadotrophin [HMG]), clomiphene citrate combined with HMG, or HMG alone. Key findings7:
- Letrozole + HMG group: Showed significantly higheroutcomes in terms of the number of mature follicles, ovulation rate, clinical pregnancy rate, and levels of estradiol and LH on the day of HMG injection. Additionally, this group demonstrated better endometrial receptivity (p<0.05).
No significant difference was observed among the three groups in abortion rates, ectopic pregnancy rates, or adverse reactions.
Therefore, the combination of letrozole and HMG was found to be the most eff ective treatment for improving ovulation and fertility in women with PCOS. It enhanced ovulation, increased the chances of pregnancy, and improved endometrial receptivity without increasing the risk of adverse effects. This approach offers a promising clinical strategy for managing ovulation and treating infertility in PCOS patients.7
Chen Y et al. investigated the optimal ovulation induction with the combination of combining letrozole, clomiphene citrate, and HMG/HMG in PCOS patients resistant to clomiphene citrate or letrozole. They included 209 PCOS patients, randomly assigned to one of three treatment groups: Clomiphene citrate + HMG, letrozole + HMG, and letrozole + clomiphene citrate. Additionally, patients who did not respond to letrozole + clomiphene citrate were treated with letrozole + clomiphene citrate + HMG. Key results8:
- The ovulation rate was significantly lower in the letrozole + clomiphene citrate group compared to the other, but similar between the clomiphene citrate + HMG, letrozole + HMG, letrozole + clomiphene citrate + HMG groups.
- The letrozole + clomiphene citrate + HMG group had higher serum estradiol levels and required more HMG, indicating a more effective ovulation induction compared to letrozole + HMG and clomiphene citrate + HMG groups.
- No severe OHSS or luteinized unruptured follicle was reported.
Combining letrozole with clomiphene citrate achieved some level of ovulation induction but adding HMG significantly improved the induction rate. The combination of letrozole, clomiphene citrate, and HMG was more effective than using letrozole with HMG or clomiphene with HMG alone, and it also lowered the chances of multiple pregnancies and OHSS.8 Weiss NS et al. in a Cochrane database systematic review found that1:
- Both HMG and recombinant FSH show similar effectiveness in women with PCOS, with no significant differences in live birth rates, multiple pregnancies, clinical pregnancy rates, or miscarriage rates, making both viable treatment options.
- Gonadotrophins lead to higher live birth rates compared to continued clomiphene citrate, without increasing the risk of multiple pregnancies.
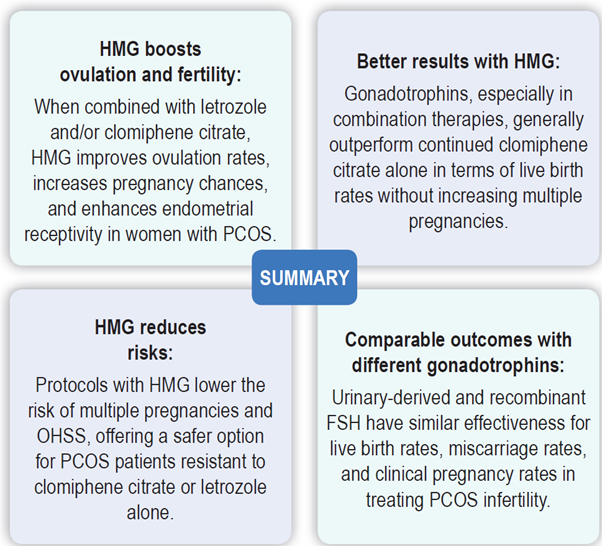
Therefore, HMG is crucial for improving ovulation and pregnancy outcomes in PCOS patients. It enhances fertility while minimizing risks, making it a highly effective option for ovulation induction.
References
1. Weiss NS, Kostova E, Nahuis M, et al. Gonadotrophins for ovulation induction in women with polycystic ovary syndrome. Cochrane Database Syst Rev. 2019; 2019(1): CD010290.
2. Tanbo T, Mellembakken J, Bjercke S, et al. Ovulation induction in polycystic ovary syndrome. AOGS. 2018; 97(10):1162–7.
3. Vyrides AA, Mahdi EE, Giannakou K. Ovulation induction techniques in women with polycystic ovary syndrome. Front Med (Lausanne). 2022; 9:982230.
4. Smithson DS, Vause TDR, Cheung AP. No. 362-Ovulation induction in polycystic ovary syndrome. J Obstet and Gynaecol Canada.2018; 40(7):978–87.
5. Yahyaei A, Vesali S, Ghaff ari F. Introduce an optimal method of ovarian stimulation in the polycystic ovarian syndrome aff ected: A randomized controlled trial. BMC Womens Health. 2023; 23: 323.
6. Jirge PR, Patil MM, Gutgutia R, et al. Ovarian stimulation in assisted reproductive technology cycles for varied patient profiles: An Indian perspective. J Hum Reprod Sci. 2022; 15(2): 112–25.
7. Xia TT, Zeng KF, Peng QM. Comparison of three ovulation induction therapies for patients with polycystic ovary syndrome and infertility. J Clin Pharmacol. 2023;63(12):1371–6.
8. Chen Y, Zhang D. Optimal ovulation induction in polycystic ovary syndrome resistant to clomiphene citrate or letrozole. Sichuan Da Xue Xue Bao Yi Xue Ban. 2016;47(6):874–7.






Comments: